How social determinants fuel cancer, cardiovascular disease deaths
CANCER AND cardiovascular disease (CVD) are the two commonest causes of morbidity and mortality in the Caribbean. Moreover, there is a growing population of patients who have both cancer and CVD, and data suggest that the economic burden faced by those with dual diagnoses is significantly higher.
Existing evidence suggests that socio-economic gradients and inequality play an important role in the incidence, treatments, and outcomes for both cancer and CVD. The conditions in the environments where people are born, live, learn, work, play, and age form social determinants of health (SDOH) that affect a wide range of health, functional and quality-of-life risks and outcomes.
The five major pillars on which SDOH are based are economic stability, educational access and quality, health care access and quality, neighbourhood build and environment and social and community context.
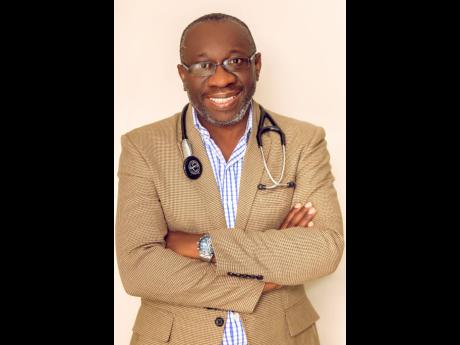
According to Dr Ernest Madu, the founder and consultant cardiologist at Heart Institute of the Caribbean, despite advances in preventive and treatment strategies for CVD, a substantial increase in the prevalence of cardiometabolic risk factors including obesity, physical inactivity, diabetes, and hypertension over the past two decades has led to a rise in premature and overall cardiometabolic mortality in the Caribbean.
“Although exponential growth in cancer and cardiovascular therapeutics has improved, overall outcomes for patients with many cancers and cardiovascular diseases, heart disease and cancer-related mortality remains prominent in rural areas, with vast urban-rural differences,” Madu said.
“Despite advances in our understanding about the impact of SDOH on cancer and CVD individually, the magnitude of their impact on patients with the dual diagnoses of cancer and CVD remains understudied,” he added.
According to statistics, at least three quarters of the world’s deaths from CVDs occur in low- and middle-income countries. People in low- and middle-income countries often do not have the benefit of integrated primary healthcare programmes for early detection and treatment of people with risk factors, compared to people in high-income countries.
People in low- and middle-income countries who suffer from CVDs and other non-communicable diseases have less access to effective and equitable healthcare services to respond to their needs. As a result, many people in low- and middle-income countries are detected late in the course of the disease and die younger from CVDs and other non-communicable diseases, often in their most productive years.
“The poorest people in low- and middle-income countries are affected most. At the household level, sufficient evidence is emerging to prove that CVDs and other non-communicable diseases contribute to poverty due to catastrophic health spending and high out-of-pocket expenditure. At macroeconomic level, CVDs place a heavy burden on the economies of low- and middle-income countries,” the cardiologist explained.
The burden of cardiovascular diseases can be reduced with cost-effective interventions. Feasible ones that can be implemented, even in low-resource settings, have been identified by WHO for prevention and control of cardiovascular diseases. They include two types of interventions: population-wide and individual, which are recommended to be used in combination to reduce the greatest cardiovascular disease burden.
Examples of population-wide interventions that can be implemented to reduce CVDs include: comprehensive tobacco control policies, taxation to reduce the intake of foods that are high in fat, sugar and salt, building walking and cycle paths to increase physical activity and strategies to reduce harmful use of alcohol and provide healthy school meals to children.
At the individual level, for prevention of first heart attacks and strokes, individual healthcare interventions need to be targeted at those with a high total cardiovascular risk, or those with single risk factor levels above traditional thresholds, such as hypertension and hypercholesterolemia.
Unfortunately, even with the most aggressive preventive interventions, many patients still will suffer from acute events, including heart attacks and strokes. A structure that does not protect the providers and patients from financial ruin limits access to many, especially the poor and the most vulnerable. In the absence of an inclusive and equitable healthcare system, many citizens will suffer adverse outcomes when confronted with acute medical illness.
keisha.hill@gleanerjm.comSOURCE: World Health Organization, Ministry of Health and Wellness, Heart Institute of the Caribbean
KEY FACTS:
• CVDs are the number one cause of death globally: more people die annually from CVDs than from any other cause.
• An estimated 17.5 million people died from CVDs in 2012, representing 31 per cent of all global deaths. Of these deaths, an estimated 7.4 million were due to coronary heart disease and 6.7 million were due to stroke.
• Over three quarters of CVD deaths take place in low- and middle-income countries.
• Out of the 16 million deaths under the age of 70 due to non-communicable diseases, 82 per cent are in low- and middle-income countries and 37 per cent are caused by CVDs.
• Most cardiovascular diseases can be prevented by addressing behavioural risk factors such as tobacco use, unhealthy diet and obesity, physical inactivity and harmful use of alcohol by using population-wide strategies.
• People with cardiovascular disease or who are at high cardiovascular risk (due to the presence of one or more risk factors such as hypertension, diabetes, hyperlipidaemia or already established disease) need early detection and management using counselling and medicines, as appropriate.