Updated | Healthcare workers say hospitals not equipped with specialised gear to deal with COVID-19
Healthcare workers say hospitals not equipped with specialised gear to deal with outbreak of the infectious disease
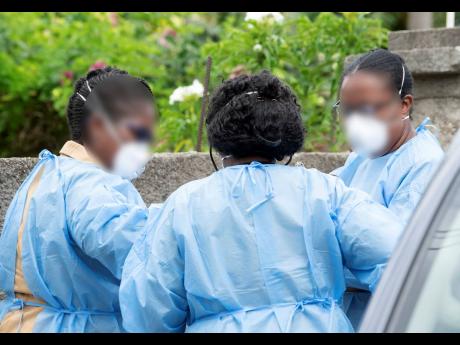
Frontline healthcare workers in the war against the dreaded coronavirus disease 2019 (COVID-19) pandemic are expressing paralysing anxiety to deal with the outbreak, as confirmed cases continue to rise in Jamaica.
Doctors and nurses stationed at several of the island’s public hospitals and clinics shared with The Sunday Gleaner that the health facilities and staff are not equipped with the specialised gear needed to treat patients afflicted with the highly infectious disease.
Up to yesterday, Jamaica had 19 laboratory-confirmed cases of COVIID-19 and was awaiting 10 results. So far, 89 persons have been tested, Minister of Health and Wellness, Dr Christopher Tufton, informed the nation on Friday.
Even as they applaud the Government’s efforts in the national dialogue, the public health workers say there is significant information deficit at the local level, noting that “there are two different realities – one at the top and one at the bottom”.
Several officials have charged that little or no information has been provided to those who are at the forefront of the fight, with no word on the required protective gear, even as they brace for an influx of coronavirus patients on an already overburdened public healthcare system.
Based on the World Health Organization (WHO) modelling, documents The Sunday Gleaner received showed that the health ministry is projecting that between 50 and 70 per cent of Jamaica’s population of approximately 2.8 million could be infected with COVID-19. The potential number of infected could be between 1.4 million and 1.9 million, with potential fatalities being 66,640 but a less aggregate of 47,600.
Senior healthcare representatives told The Sunday Gleaner that the sector will take a “massive hit” because first contact personnel cannot protect themselves.
According to them, for far too long hospitals have been hiding under the Personal Protective Equipment (PPE) shield, telling workers that they have protective gear, but they are not the proper ones designed to adequately safeguard healthcare providers in the face of a dreaded infectious disease such as COVID-19.
They said many first responders have not been fitted or issued with the WHO recommended N95 respirators and surgical masks or the hazmat suits, which are critical to dealing with COVID-19 that has now infected some 182 countries, with approximately 266,073 cases and an estimated 11,184 deaths. The novel coronavirus was first detected in China in December last year.
‘GOING TO DIE’
“We have been asking for weeks. Months. When we heard that the coronavirus broke out in China, we kept on asking what are we going to do. Jamaica and China business is almost like the USA and us. So it was just a matter of time before it reached us. But everyone was just hoping it away,” said a senior medical professional with more than 30 years’ experience, who asked not to be named.
The Kingston Public Hospital (KPH), they believe, would be the worst hit, stressing that doctors and nurses there were “going to die”.
“Anyone who works in the public hospitals’ accident and emergency units will be in grave danger,” said another.
“Everyone should have been fitted with the protective gear from the first of March. Then have them tested for leaks to make sure that in treating the patients, they do not become contaminated.”
However, Wentworth Charles, chairman of the South East Regional Health Authority (SERHA), which represents nine hospitals and more than 90 clinics in Kingston, St Andrew, St Thomas, and St Catherine, told The Sunday Gleaner that, “the region is not short of personal protective equipment. All institutions in SERHA have enough supplies and we have ordered more through the National Health Fund. These include masks, surgical masks, gloves, etc. The hazmat suits have not been issued but are with SERHA.”
He added that the “suits must be fitted, then the individuals placed in a room and liquid sprayed for smell test. If there is a smell or any fluid inside the suit, then there is a leak so it has to be discarded.”
Charles stressed, “We have to protect the people on whose backs the sector rests.”
FITTING FOR TUESDAY
On Friday evening, The Sunday Gleaner was sent a copy of a letter that was dispatched by the Ministry of Health & Wellness, which stated that on Tuesday, March 24, thirty persons were scheduled for mask fit testing. Sixteen of the personnel are from KPH.
With more than 200 persons in COVID-19 isolation facilities in SERHA, including hospitals, Prime Minister Andrew Holness, during his Budget presentation last week, warned that, like other countries, Jamaica needs to brace for a surge in cases.
“From the data, and looking at the experience of other countries, it is my duty to prepare the minds of the Jamaican people to understand that cases of COVID-19 will increase, and there may be even instances of rapid increase,” he said.
The Jamaica Medical Doctors Association (JMDA), which represents junior doctors, also expressed “grave concerns about readiness”.
“I don’t think anyone feels ready in the hospitals. Practically, we have grave concerns. But I am reassuring them and making representations at the national and local levels with respect to their concerns,” said President Dr Elon Thompson.
On Tuesday, during a virtual town hall meeting hosted by Television Jamaica, Thompson said nurses and medical interns were often “human ventilators”, assisting patients to breathe by squeezing the bag in human breathing motion. That, he said, will hastily become a thing of the past if there was a flood of persons needing respiratory assistance and intensive care from COVID-19, which is a respiratory disease.
Dr Thompson said Jamaica’s medical doctors were among the best trained in the hemisphere but could achieve so much more with just a little more.
CRISIS OF ‘UNSEEN DARK PROPORTIONS’
Nurses Association of Jamaica president, Carmen Johnson, said up to Friday they were aware that a team of individuals were fitting medical professionals with protective gear.
“They were fitting accident and emergency personnel and the areas that are likely to be the first point of contact with infected persons. Not all persons were fitted because some did not make themselves available for various reasons. In my view, it should have been a mandatory fitting,” she told The Sunday Gleaner.
“We have not yet seen the hazmat suits although we know that is what is required. To say we have gotten them, no. None of my nurses up today (Friday).”
She also shared that bathrooms that were once discarded in some institutions are now being retrofitted to allow nurses to shower after duties. Nurses are also now dressing for work, at work. They are also encouraged to wear disposable uniforms, including gowns and pants, but some personnel have complained that those are woefully inadequate in the fight against dreaded diseases such as COVID-19.
A senior medical doctor at the Cornwall Regional Hospital in St James said a crisis of “unseen dark proportions” could break out at the hospital.
“Because of the situation there with the refurbishing – which is a huge and commendable effort and should be named after the minister when it is done – but that aside, the patients’ beds are so close that you can reach across and touch someone,” said the doctor. “Every doctor and nurse there should be honoured.”
Adding their voice to the concerns, one porter said they were “one group in the sector who no one cares about. All I have is a uniform and regular mask.”
Sunday Gleaner checks with 14 clinics in Kingston, St Andrew, St Thomas, St Catherine, Manchester and St Elizabeth revealed that medical professionals were in need of the proper protective gear.
MILLIONS ALLOCATED
In the meantime, Prime Minister Holness has moved to allay fears in the public health sector about the lack of appropriate safeguards to treat COVID-19 patients, by announcing that the Government had secured 400,000 N95 masks and other personal protective equipment for healthcare workers.
Holness said that his administration has spent $547 million to procure drugs for the treatment of COVID-19 and that the Government would spend more than $150 million to develop new quarantine facilities to house an additional 150 persons.
He added that more than $287 million was being spent to retrofit public hospitals and health facilities to accommodate patients during the peak of the epidemic. And another $198 million is being spent to acquire ventilators for the high-dependency units in various hospitals.
The Government has also allocated $25 billion of the 2020-2021 Budget for economic stimulus to aid with the fallout from the public health crisis.
The Private Sector Organisation of Jamaica has also committed $150 million to the Government, to aid in the COVID-19 fight.
NOTE: An earlier version of this story had quoted the Health Minister in an interview with The Sunday Gleaner as saying frontline workers including doctors and nurses had tested positive for the coronavirus. The ministry has since clarified that position saying no frontline worker has tested positive.