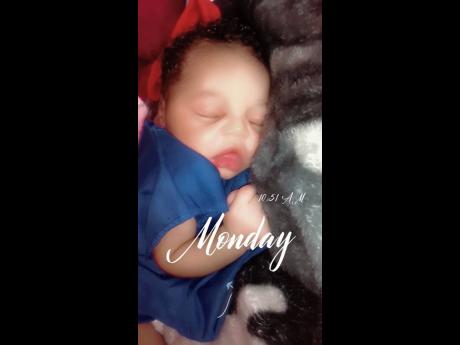
‘I sat there with my dead baby in my hand’
- Mother trying to cope with death of daughter two days after birth - Black River Hospital implements new protocol for newborns as probe continues into Baby Akira’s death
A baby’s death two days after being born has triggered a mandatory requirement for all newborns at the Black River Hospital in St Elizabeth to be seen any day of the week by a member of the paediatric unit before being discharged. Shakera Morgan,...
A baby’s death two days after being born has triggered a mandatory requirement for all newborns at the Black River Hospital in St Elizabeth to be seen any day of the week by a member of the paediatric unit before being discharged.
Shakera Morgan, 29, now wonders whether her daughter Akira Campbell, her second child, would have been alive today if that rule was implemented before they were discharged on Sunday, January 29, a day after she was admitted and later gave birth.
“The baby was not seen by a paediatrician prior to discharge – there is less staff on the weekends,” the hospital’s Chief Executive Officer Diana Brown-Miller told The Sunday Gleaner, adding that “although not a national policy, on a weekday, every newborn is seen by a member of the paediatric team prior to discharge”.
But, since Akira’s death on January 31, the protocol at the hospital has changed to include weekends.
“We have now instituted a system where staff from the paediatric unit sees all babies, regardless of the day of the week,” Brown-Miller told The Sunday Gleaner in responses provided on March 7.
But, even before the hospital concludes its investigation into the matter, the public institution’s boss made it clear that “within the constraints of our operations, the institution delivered” and “the mother received standard care in keeping with national guidelines. There were no gaps in treatment of mother and baby”.
“On discharge, the baby was reviewed by a midwife and team on the maternity ward and vital signs were normal,” she said, pointing to the baby’s oxygen saturation, heart rate, respiration and temperature. The mother’s vitals were also reported as normal.
Questions submitted on March 9 to the Ministry of Health and Wellness on broad policy and resource issues surrounding the care of newborns in public institutions’ paediatric care remain unanswered.
‘How long she stop breathe?’
Morgan has claimed that, before being discharged, her baby “didn’t see a paediatrician nor [was] examined by a nurse”. She said an official at the hospital gave her a note which said she was to return with the baby at 8:30 a.m. on Tuesday, January 31.
“Before I get the paper, I was there on the bed and I realise that my baby sound stuffy. So, I called to the doctor and I said ‘Doc, I don’t like how mi baby sound’. He came, he put his ears over the baby’s nose and he turned to me and said I can get a nose drop at the pharmacy … and he discharged me,” she said.
She said she did not get to buy the nose drop because there was no pharmacy open on Sunday.
Morgan went home with Akira on January 29 and, during that time up to the morning of January 31, “mi never did a see me baby sickout or show any kind of reaction to anything”.
On the morning of January 31, as Morgan headed to the bathroom in preparation to leave for the hospital, her sister with whom she lives in Mount Pleasant, sensed something.
“Mi sister call me back and seh mi fi come because she nuh like how the baby a breathe. So, I went in the room and me realise that something was wrong with my child but I couldn’t state what was wrong. So I rushed to the hospital (Black River) with the baby,” she recounted.
She arrived at the hospital’s Accident and Emergency (A&E) Department where a doctor reportedly took the baby after several appeals for help. Morgan said she stayed in the waiting area “for a good while”.
“Everybody come out, mi ask ‘wah a gwaan wid me baby?’ Nobody answered me. Okay. I sat there patiently waiting and hoping and praying to God fi just mek mi baby alright,” she said.
Hours later, she said a nurse took her into a room where other officials were already.
There she saw baby Akira on a bed.
“Mi seh ‘the baby nah breathe?’ Nobody answered … so I went and I put my finger underneath the baby’s nose I realised mi baby nah breathe. So, mi seh ‘How long now since mi baby stop breathe?’ Nobody answered me,” Morgan said.
Baby Akira was dead. Just a week before her mother’s birthday on February 7.
‘Where is
my baby?’
Morgan said she was advised to await the arrival of the police. And, for another few hours, “I sat there in the chair with my dead baby in my hand”.
The police turned up, took her name and other information and then told her that the body would have to be taken to a funeral home. She also queried whether a private autopsy could be done.
All that time, Morgan said she continued to sit with the body because “I’m not going to move until I see which funeral home is taking my child”.
Her sister, who had joined her by then, received a phone call from a hospital official who told Morgan that she was needed for further discussions.
Morgan said, for an additional two hours, she did not move until the female official she said she spoke with came to the room and invited her to a “private conversation” with other officials.
“I was walking behind her with the baby and she seh to me I cannot take the baby with me. So me seh ‘me haffi guh leave me baby?’ She said ‘Yes’. Me ask ‘So, when me leff my baby pon the bed, me a come back here so come see har?’ I find it hard to put down my child,” she said of further talks with the official.
Morgan said she left the body on the bed and accompanied the official to a room with seven hospital personnel. Her sister and family friend went with her.
She said the officials questioned her about the baby’s birth and the hospital discharge process.
During the discussions, one of the officials reportedly got a call that a team from the funeral home had arrived. Morgan told the woman she wanted to accompany her back to the A&E room where she left the baby Akira’s body.
“First place I look on the bed where I left my dead child and she not there. So, me see di security so me seh ‘weh me baby deh weh mi leff ya so?’ Security nuh ansa me. So, me seh ‘weh mi baby weh mi leff pon the bed ya so?’ Nobody don’t answer me. The lady asked where is the child, and dem seh [a] funeral home took the child.”
Brown-Miller, the hospital’s chief executive officer, said she could not confirm what killed Akira because the police “had an interest” in the body. But she said the baby “is noted in the records of Accident and Emergency as a death on arrival”.
Given that the child was only pronounced dead at the hospital, protocol required the police to be informed for them to rule out any foul play through a post-mortem, after which the family would be allowed to take the body.
‘Congenital pneumonia’ cause of death
After weeks of back and forth with the hospital, the police and funeral home, an autopsy was done on February 27, with the cause of death noted on the police-signed death certificate as “congenital pneumonia”.
The word ‘congenital’ means a condition that is in existence at birth, so a congenital pneumonia is an infection in the lungs that is present at the time of birth, explained Dr Brian James, a consultant anaesthetist and intensivist at the Bustamante Hospital for Children in St Andrew.
“The implication of it is that it was contracted either in the womb during the latter part of the pregnancy or around the time of birth. Because pneumonia is something that actually develops over a few days, most times it is not contracted during the birth passage, it is contracted before,” he said, noting that it is treated like regular pneumonia cases with antibiotics and respiratory support.
In her March response, the Black River Hospital’s boss reiterated that there were no red flags before the mother and her baby were cleared for release.
“There was no clinical indication of any infection prior to discharge. No cough, shortness of breath, cyanosis, vomiting, fever or poor feeding … vitals were normal and so, too, the feed pattern,” Brown-Miller explained.
Cyanosis is the blueish discolouration of skin because of a lack of oxygen.
Before Akira’s death, “newborns delivered on weekends were brought back for paediatric review on the Tuesday following discharge,” explained Brown-Miller, who said the Black River Hospital is now “one of the first hospitals in the island that attempts to see all babies prior to discharge, despite this not being a national policy on the weekday”.
No money for lawyer
Morgan, who observed the autopsy in Kingston, said the pathologist used information from her file submitted by the hospital to question whether she was advised that she got an infection after giving birth and that the child had an infection on her lungs from birth.
“Nobody told me about nuh infection and nobody treated me for infection there, so why is that in my docket?” Morgan said she told the pathologist.
Morgan said her baby was due the February 5 and she visited the Malvern Health Centre every month until November when her check-ups were every two weeks. She said she was never diagnosed with an infection.
Yesterday, Brown-Miller told The Sunday Gleaner that she could not immediately speak to what was recorded on Morgan’s file.
On Friday, the CEO indicated that the investigation into a complaint that Morgan filed on March 1 was still ongoing.
“Yes … but I don’t have the money to put a lawyer on it,” said Morgan, who is currently unemployed, when asked whether she has contemplated seeking legal advice.
Black River Hospital is a Type C institution, the lowest designation for a government hospital.
Those institutions have between 60 and 95 beds and provide primary-care services and basic secondary-care services. They have fewer specialists on staff and therefore limited inpatient and outpatient services.
Resource challenges
Dr James, who is also the president of the Medical Association of Jamaica, said what happens when a baby is born in Jamaica’s public institutions depends on the type of hospital in which the delivery takes place.
“Those hospitals that do not have a paediatrician, they are checked by the midwife who is doing the delivery,” he said, speaking generally of Type C institutions, which he said are associated with hospitals with higher designations and therefore access to a paediatrician.
A midwife is a person trained and certified to, among other things, conduct births, provide care for the newborns and mothers, and detect complications in mother and child, according to the International Confederation of Midwives.
James explained that, when there’s reference to ‘paediatrician’, “it doesn’t mean a specialist paediatrician, it means paediatric staff, so that it would be a resident doctor who would see those patients on the post-natal ward and, if there are issues, then they would refer it up the chain until it gets to a paediatrician”.
The medical consultant said, ideally, a newborn should be seen by a physician, such as what happens in private practice.
But getting to that ideal in the public system may be problematic for Jamaica, given the general shortage of healthcare practitioners.
“We are certainly below the recommended levels, so, using those figures, there is a shortage. I don’t think paediatricians are outside of that particular data set. There’s a shortage of just about every kind of healthcare professional,” said the former head of the Department of Anesthesia and Intensive Care at the Bustamante Hospital for Children.
Jamaica’s density ratio of 2.71 doctors and nurses per 1,000 population is below the minimum density ratio of 4.45 skilled healthcare workers recommended by the World Health Organization, the Auditor General’s Department reported in March.