Mental misery
The hidden struggles of men and mental health in Jamaica
Relatives of Shankar Maragh are worried sick. They have not seen the 36-year-old, a deportee from the United States who battles mental illness, since April 2020. They hope he is still alive; his twin sister Shakeera is the most faithful, but with every month that passes, that hope dwindles.
Maragh, who migrated to the US as a child, struggled with marijuana abuse, and various drug-related infractions in the US landed him before the courts and, ultimately, caused his deportation, Shakeera explained.
Shunned by both sides of his parents’ families – as is the case of many deportees – Maragh ended up at a family friend’s home in St Catherine. However, that family friend died shortly after. That’s when things took a turn for the worst, Shakeera said.
“He went into an environment with a lot of drugs and it wasn’t a good place for him to be,” a shattered Shakeera said during a telephone interview with The Sunday Gleaner from the US last week.
“There was a lot of drinking and smoking, and he wasn’t supposed to be around that,” she stressed, adding that some time after, there was reportedly a conflict that led to her brother leaving the premises.
“He left his wallet, his phone, everything was on the bed, but we can’t find him. The next day, we heard that he was in Kingston. We don’t know how he got to Kingston from St Catherine,” she said worriedly. “A neighbour said he saw my brother in shorts, broken-down shoes, and he didn’t look good.
“My brother isn’t like that, he is always really dressed up and put together.” Shakeera said her brother, who was reportedly incoherent, told the neighbour he was on his way to check on somebody and walked away. “They took a video of him walking away, and that was the only video of him we have in Kingston.
“So after that sighting, we are encouraged that he is still alive,” Shakeera stressed, hoping somebody knows his whereabouts, even though the video with her brother is four years old.
Shakeera said her brother was on medication for mental issues before his deportation.
WALKING THE STREETS
Their stories vary, and so, too, do their specific mental health issues; and while more females are afflicted, according to research, males often play out their realities more violently. Experts say the strains tend to come from work-related issues, financial shortcomings, divorces and custody battles, and a general feeling of unworthiness. And as men are also slower to seek help and stick to their medication, their situations are further complicated.
Today is the last day of Male Mental Health Awareness Month, celebrated in June.
“Mental health issues generally occur more in women than men. But the big issue is that men are poor seekers of health, for physical health, and worse, for mental health,” outlined Dr Kevin Goulbourne, director of mental health and substance abuse in the Mental Health Unit of the Ministry of Health and Wellness.
“Also, men have poor support systems around them. Women will bond to each other but men are not so close as it relates to sharing their problems and personal stories. Therefore, men use more unhealthy ways to cope with stress,” he outlined, listing gambling and alcohol drinking while underscoring the negative reinforcement of Jamaica’s social norms on men.
“So ego and pride get in the way of them seeking help, and also, medication that is given for mental illness will harm their manhood. So even if they are diagnosed, they would be less likely to take the medication,” Goulbourne continued, citing stats from the Jamaica Health and Lifestyle Survey (2017), which estimated depressive disorder in Jamaican men at 9.9 per cent in males and 18.5 per cent in females.
Some 160 persons reportedly attempted suicide in 2017, Goulbourne said, for example, and up to 70 per cent of them were females. On the flip side, however, more males have killed themselves than females in any one year; and the studies have also pointed to the younger males – between 18 and 29 – who are attempting suicide, Goulbourne explained.
Between January 2021 and May this year, there were some 8,286 calls to the mental health and suicide helpline set up by the Ministry of Health. The highest number of calls (484) to the hotline came in October 2022, followed by July 2023, with 334 calls. A total of 1,866 men have called the hotline over the period, in comparison to 4,927 females – some of whom may have been calling on behalf of male counterparts.
Depression leads the local mental health cases when it comes to men, said Goulbourne, citing anxiety, bipolar disorder (manic depressive illnesses), substance abuse disorder, ganja, and nicotine use disorder, he explained, pointing to the decriminalisation of marijuana and the proliferation of vaping among some of the other causal factors for what seems to be a trend.
GAMBLING DISORDERS
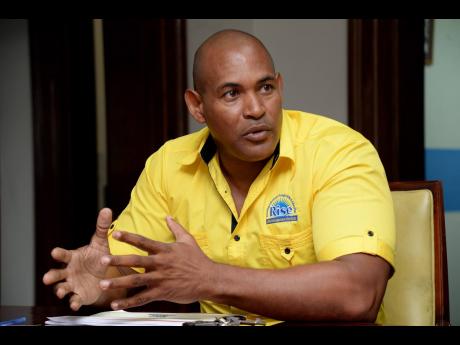
Other issues affecting male mental health in Jamaica are gambling disorders, which Richard Henry, head of gambling counselling and support services at RISE Life Management Services, believes often start in the home and school community environment before years later manifesting into greater mental health problems for Jamaican men.
“Gambling disorders in men can lead to critical problematic issues. These include mental health issues such as depression, anxiety, personality disorders, and severe financial strain, as well as damaged interpersonal relationships and familial issues,” Henry said, also noting psychological issues regarding low self-esteem, a sense of worthlessness, skewed values, and unachieved goals.
There is also a strong link between male gambling addiction and suicide, he noted, further underscoring that RISE treated 290 school-based youth with gambling addiction and all of them were males. The data shows a vast disparity between male students who gamble and female students, he said, even though the consequences of gambling for females may result in sexual exploitation that could have lifelong implications, according to some educators.
“The data has already confirmed for us that men are less likely to seek medical support than women, hence the increased possibility of extreme actions,” Henry noted, underscoring some of the behavioural issues that are manifesting in young boys across the country.
GAPS REMAIN
In the meantime, Najuequa Barnes, a data privacy and corporate consultant, has advocated for mental health services for men in Jamaica through a robust regulatory framework.
Barnes told The Sunday Gleaner that while Jamaica’s mental health offerings have improved significantly over decades, there are still gaps that need to be bridged by beating down stereotypes and catering for men suffering from mental health issues through the legal system.
“The Mental Health Act of 1997 is the cornerstone of Jamaica’s mental health legislation, outlining the rights of patients and the responsibilities of mental health facilities. Despite its importance, the act is outdated and lacks provisions to address contemporary mental health challenges, especially those faced by males,” Barnes argued.
“The act needs revision to incorporate gender-sensitive approaches and modern treatment modalities, reflecting current best practices in mental health care,” she continued. “One significant gap is the lack of targeted mental health services for males in rural areas. Access to mental health care is predominantly urban-centric, leaving rural men without adequate support.”