Christmas concern
Health sector bracing for fourth COVID-19 wave; road accidents causing jitters for holidays
Health officials are hoping that the island will be able to delay an expected fourth wave of the COVID-19 pandemic to give the sector more breathing space to recover from the devastating third hit, but administrators are still nervously anticipating the traditional increase in the number of road and home accidents that characterise the Yuletide season.
With relaxation of the nightly curfew contracted by one hour for the season – and starting much later on the traditional grand market night and to ring in the new year – more Jamaicans are expected to be on the road making merry, prompting the health ministry to urge extra vigilance, including adhering to COVID-19 protocols.
It is also not taking for granted the declining hospitalisation and positivity rate of COVID patients. Up to Friday, Jamaica recorded an overall 91,725 COVID-19 cases and 2,424 deaths. With 73 positive cases in a 24-hour period, the positivity rate stood at seven per cent with 124 persons hospitalised.
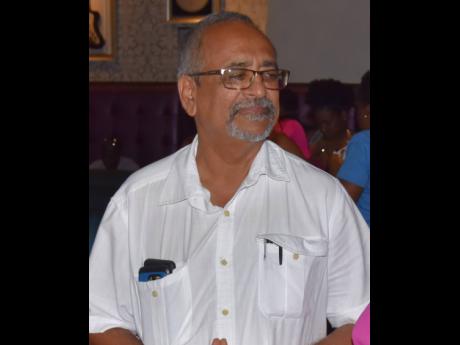
“This is the season for most motor vehicle and house accidents and, on the tail end, is the impending arrival of the fourth wave of the coronavirus. We are constantly planning for these eventualities. We know what to expect when it comes to the festive season, so, therefore, we have looked at our staffing to make sure we have adequate coverage, especially for the accident and emergency departments, which have to be optimum 24 hours, along with our equipment, to make sure everything is up and running to the best of our abilities,” said Errol Greene, regional director of the South Eastern Regional Health Authority (SERHA), which has 15 institutions under its management.
“Our main focus this year, however, is preparation for the onslaught of the fourth wave which might hit us. We have looked at our hospital capacity, how we can expand the bed capacity, and, even as we speak, some of our hospitals have high occupancy with non-COVID patients,” he added.
“For our COVID facilities, we have a 40-bed field hospital in Spanish Town, which is not occupied now, but we are prepared to press it into service if needs be. We have looked at other wards at the Spanish Town Hospital. We have completed piping for oxygen so we have oxygen from bulk storage rather than depend on cylinders.
“At National Chest in [St Andrew], piping has also been completed on the wards, bulk [oxygen] storage capacity is also in place, and bed space and triage areas are also in place,” Greene added.
CHALLENGES
He, however, noted that there were challenges to the supply of oxygen to the Princess Margaret Hospital in St Thomas.
“Our supplier has told us that when a unit is sent to that hospital, it takes an entire day from Ferry [in St Catherine] to Princess Margaret because of ongoing road development in the area. So we have looked at increasing cylinder capacity so they can store more and make less trips,” he said.
During the third wave of COVID-19 in the summer, overcapacity at hospitals led to dire shortage of medical-grade oxygen. However, both the Government and sole-supplier Industrial Gases Limited (IGL) recently assured that adequate supplies of the life-saving commodity will be available, if and when needed.
According to Greene, among the occupants of hospitals are social patients who have been dumped on health facilities islandwide by relatives. Greene is pleading with families to collect their relatives.
The 40-bed St Joseph’s Hospital in Vineyard Town, Kingston, was housing 11 patients up to Friday who were non-COVID cases.
“If the relatives could cooperate with us, so we can free up the bed space, that would be good. Fifty per cent of the bed capacity at Linstead Hospital are also social patients, so we have a challenge there as well. But we are coping with it the best ways we can,” he said.
The CEO of SERHA was also confident that there was enough personal protective equipment (PPE) for medical personnel.
“We are having a challenge with recruitment, especially as it relates to doctors. We can’t offer them a two- or three-year contract. The recruitment is just to deal with an emergency and most doctors are reluctant to take a six-month contract, which is what we can offer at this time. That is posing a challenge,” he disclosed.
Nurses are also short.
“We are short, because nurses are migrating. Every month, we get the numbers who have left. The experienced nurses are leaving. We are trying to encourage those who stay with training opportunities in specialised areas. Some persons are taking it up, but we are not satisfied with the level of responses that we are seeing. For example, nurse anaesthetist is a function that is very critical to the sector. I have personally suggested to my region that I will ask the board to support the training for these individuals, but the take-up is not good,” Greene shared.
Further challenges include the shutdown of the Edwina Ward at the Kingston Public Hospital (KPH) because of structural damage. Patients were relocated.
“We continue to monitor the situation there, but it has put a strain on the capacity and it is not something that is going to be fixed easily, because we also have issues with termites, and the infrastructure is in a state of disrepair on that ward. We have to gut it and rebuild it,” he disclosed.
Greene expressed gratitude to corporate Jamaica for its support of front-line workers.
BE VIGILANT
Clinical coordinator for the Western Regional Health Authority (WRHA), Dr Delroy Fray, said COVID-19 numbers were down for facilities in that section of the island.
“Up to Friday, when I checked my data of the hospitals around, we have been doing well. Sav-la-mar Hospital had five patients, Noel Holmes had one, Cornwall Regional Hospital had about 10 to 13, and the numbers are also down at Falmouth. So what we are seeing as we go into the Christmas season, the numbers are down and we are hoping that it stays that way,” Fray told The Sunday Gleaner yesterday. “But we cannot become complacent. We have to be vigilant to ensure that once we go into the new year, we will not have a sudden rise in cases.”
Fray continued: “We are not saying you are not to go out, because what I am seeing is a lot of emotional disturbance based on the restrictions, and it involves a lot of young people. What we are saying is that you can go out, but make sure that the congregations are small. Still wear your mask, still sanitise and do what you have to do to protect yourself.”
Through a private sector effort, the University Hospital of the West Indies (UHWI) recently received containers that were reconfigured into hospital rooms, giving the facility additional space to treat patients.
“We call them holding wards. You get admitted and treated until the regular hospital has free beds. However, it is above the standard of field hospital tents. It is air-conditioned, has video physiological surveillance monitoring, bathrooms, nurses’ station, donning and doffing and two separate resuscitation rooms,” said Dr Carl Bruce, UHWI’s medical chief of staff.
The reconfigured containers have added 35-40 rooms, and with space for an additional four modular units, and 50 to 60 patients can be accommodated, he said.
According to Bruce, the plan is to use the facility for non-COVID patients, who are overwhelming the hospital currently, and “switch back when COVID numbers rise again”.
COMMITTED TO THE TASK
Health Minister Dr Christopher Tufton said the Government was doing everything it can in anticipation of a fourth wave of the virus.
“In preparation for the fourth wave, we are currently building out a field hospital at Savanna-la-Mar. We are also discussing oxygen supplies and should be prepared based on what the sole supplier says. There is adequate supply of PPEs and more is being put in place. The greatest part, however, is that doctors and nurses in the system remain committed to their task,” Tufton told The Sunday Gleaner yesterday.
He said field hospitals were at May Pen, UHWI, St Joseph’s, Spanish Town and Falmouth health institutions, adding that some of the facilities were empty.
Urging caution for the Yuletide season, Tufton said, “It is important that Jamaicans continue to take special care to protect themselves and family during the season. As we say, Christmas is not cancelled despite COVID. Whatever we do with family and friends, observe the protocols. Be extremely careful on the roads, don’t overindulge, get rest and enjoy quiet time with family and friends.”
‘SLOW DOWN’
Vice chair of the National Road Safety Council, Dr Lucien Jones, said his message was simple.
“Slow down. Today (Saturday) we are at 440 road fatalities. The whole year is a season for road accidents, not just Christmas. And the message for all times is to slow down. The data coming out of the World Health Organization is that a five per cent reduction in average speed translates to 30 per cent reduction in fatalities. That’s all you need. The slower you drive, the more lives you are likely to save,” said Jones yesterday.
He said the nation can be galvanised around the Road Traffic Act, which has a number of effective provisions.
“Cut down your speed,” he again pleaded.
Each official urged Jamaicans not yet vaccinated to do so, as there was no shortage of vaccines. Vulnerable individuals who meet the criteria are also advised to take the flu shot.